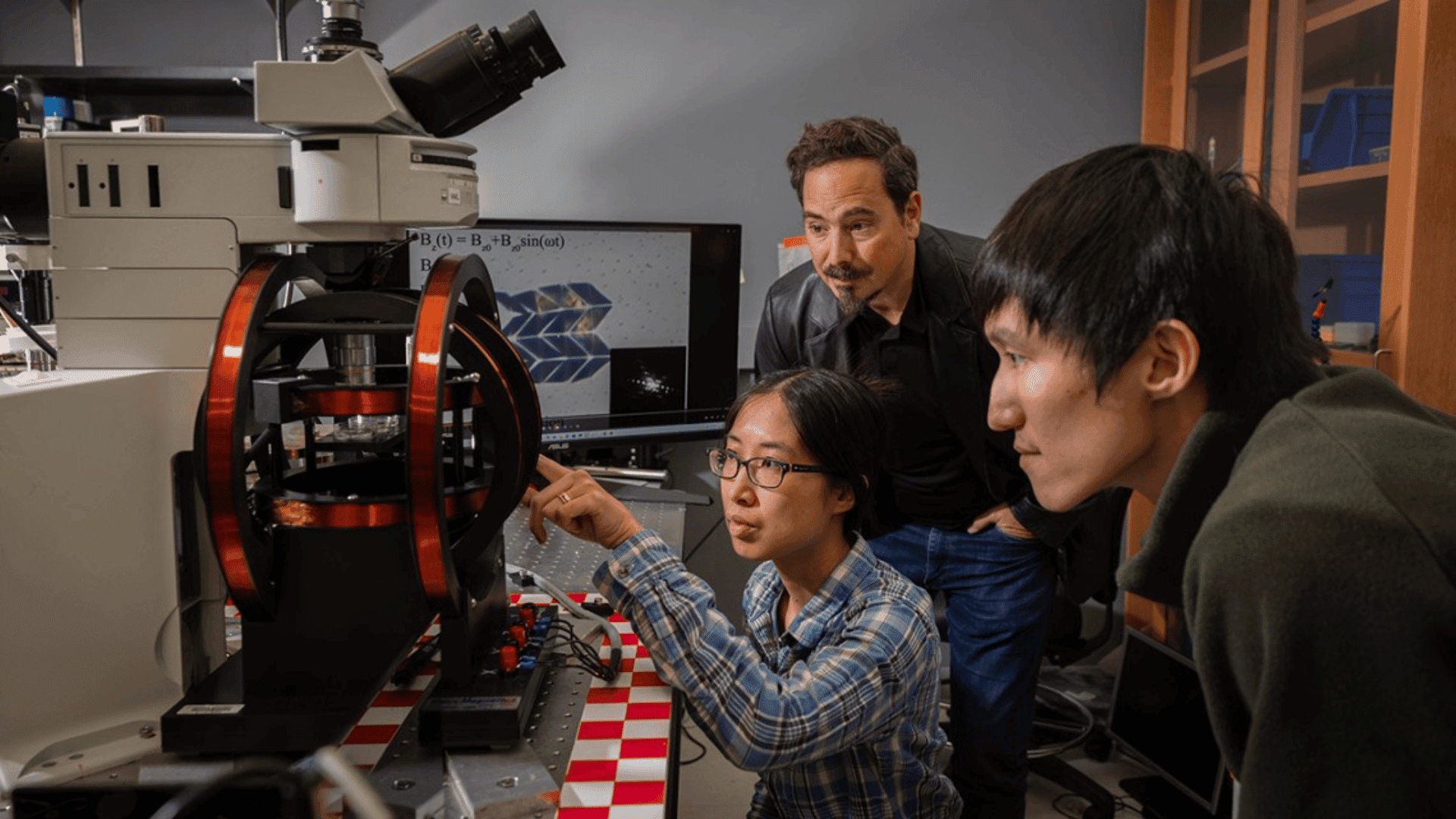
A new and innovative amputation surgery has been making headlines and giving amputees a new lease on life. Developed by MIT researchers in collaboration with surgeons at Harvard Medical School, the surgery allows amputees to better control their residual muscles and receive sensory feedback. In most amputation surgeries, muscle pairs that control affected joints are severed. The MIT Team, however, has found that by reconnecting these muscle pairs, it allows the amputee to receive much better sensory feedback. This has led to amputees gaining better control of robotic prosthetics and a reduction of ‘phantom limb’ pain.
We were able to speak with Dr. Shriya Srinivasan, MIT postdoc and lead author of this study, to learn more about her work.

Tomorrow’s World Today (TWT): What inspired you to pursue biomedical engineering?
Dr. Shriya Srinivasan (SS): I volunteered for various clinics when I was PreMed and I saw a lot of health disparities around different clinics, especially in Cleveland. For example, when I’d volunteered at the free clinic of Greater Cleveland as well as Cleveland Clinic, the disparities in care and access to technology were apparent. . And for a lot of the practical limitations, my mind very quickly drew parallels between the technological advancements that we have and the clinical needs. I thought there are so many gaps that could easily be bridged with the technology we have today. So it was that experience that inspired me to move towards biomedical engineering.
TWT: What was the most challenging part of your research? How did you overcome it?
SS: When you first get started on a problem, there are many years ahead of you in the problem-solving process and you don’t know if the solution you’re proposing is going to work. So dealing with that uncertainty was the most challenging part for me. At first, I think that was a very daunting feeling, knowing that you’re coming up with something completely new, likely to have components that aren’t going to work and require troubleshooting. How did I overcome it? I guess just persistence, falling down a lot and getting back up, and knowing that’s just part of the process.
TWT: What was the most rewarding part?
SS: The most rewarding part has been working with the patients that had undergone the AMI amputation. Many returned to sports, hiking, and playing outside with their kids after many years of being immobile. In the lab, they were able to report much better sensations and comfort of the limb, and these were very meaningful to hear and witness.
TWT: And this technique works for both people who are new amputees and those who previously had a different amputation surgery?
SS: That’s right, the AMI amputation can be performed using native muscle or small muscle grafts if someone’s already had an amputation. It’s one of the few techniques that you could use on somebody who has already had an amputation to enable this type of functionality. This allows them to “upgrade” their neuromuscular anatomy to better interface with the advanced robotic limbs that we have today.

TWT: Who are your personal or professional role models?
SS: This is a hard question because there are so many. Many professors I’ve worked with, both at Harvard Medical School and at MIT have been critically inspiring role models. Not only from their approach to science and approach of questions but also the way they lead their lives and interact with students and patients is remarkable. Given their impact in the field, it is humbling to work alongside them.
TWT: What’s next for you?
SS: I’m currently doing a postdoc, research neuromodulation in the GI tract. There has been a considerable buzz around gut health and the connection between the brain and the gut, but few interventions on the neural level. I’m interested in communicating with the nervous system in the GI system towards improving GI diseases. After that, I hope to find a faculty position and run a lab that develops translational medical devices.
TWT: You are also a professional dancer. Has your study of dance influenced your work? If so, how?
SS: Yes, it has. While learning and performing dance, you perform an intimate study of movement. The body learns to plan turns and jumps with just the right amount of force to achieve a given effect. “If I do this turn with this much speed, I’m going to land here.” When I started studying biomechanics, physiology, and anatomy, the intuition developed from my dance training lent itself to an integrated understanding of each component.
I now teach a course called Biomechanics in Bharatanatyam, Bharatanatyam is the name of this Indian classical dance form that I pursue. It teaches dancers how to think of their bodies from a physiology and anatomy perspective and incorporate those principles into their dance.
TWT: Why do you think it’s been nearly 200 years since any major changes have been made in the field of amputations?
SS: There have been advances in the last 10-15 years, but none of them have fundamentally addressed the challenge of returning sensory feedback to the body. Historically the fields of engineering, rehabilitation, prosthetics, and surgery have been siloed. Surgeons operated in hospitals, engineers built robots in labs, prosthetists outfitted patients in their own clinics, and so on – with little overlap between the spheres. The interdisciplinary approach we took restructured this framework.
It’s also possible that the technology wasn’t primed to such a degree that we started to see the gap in amputation. But now bionics have pushed ahead so much that the lack of advances in surgery became apparent.
I think it’s a combination of these factors, but if I had to bet on one, it’s that such interdisciplinary science has not been done with such efficiency before.

TWT: What do you believe is the future for amputation surgery and research?
SS: Customization of surgical approach to each person’s anatomy and prosthetic needs will be furthered given current trends. A patient’s muscles and bone structure could be imaged pre-operatively and folded into plans for their postoperative prosthesis preferences, directing the types of functionality that are built into their residuum. Smart sensing and actuation technologies will also find themselves at the center of implants, prosthetics, and surgery. In 50-60 years, I think it’s possible that one could have implanted robotics joints.
TWT: What type of progress are you hoping to see in the field of amputation surgery and prosthetics in the next decade?
SS: I would hope to see more, my advisor likes to call it, ‘human embodied design’ or design that is more human-centered and incorporates the nervous system, design that seamlessly interacts with our body.
I also hope that the issues of access are also seriously addressed. Today, most prosthetics are far too expensive for people in the developing world to afford, where a large proportion of people with amputations reside. Consequently, many use wheelchairs or crutches as a permanent solution. Developing new prostheses that are fundamentally focused on access and affordability would be a game-changer for many societies.
TWT: Since you had mentioned you were working on innovations in gut health, what sort of advances are you hoping to see in that field over the next decade or so?
SS: I envision a future in which people swallow smart pills that can sense and track the health of the GI tract, map out changing microbiome data in the intestines, and help people proactively eat healthily and maintain their weight or manage their diseases. With a more data-driven approach, device-based innovation for the GI systems could modify behavior and enable people to lead disease-free lives.