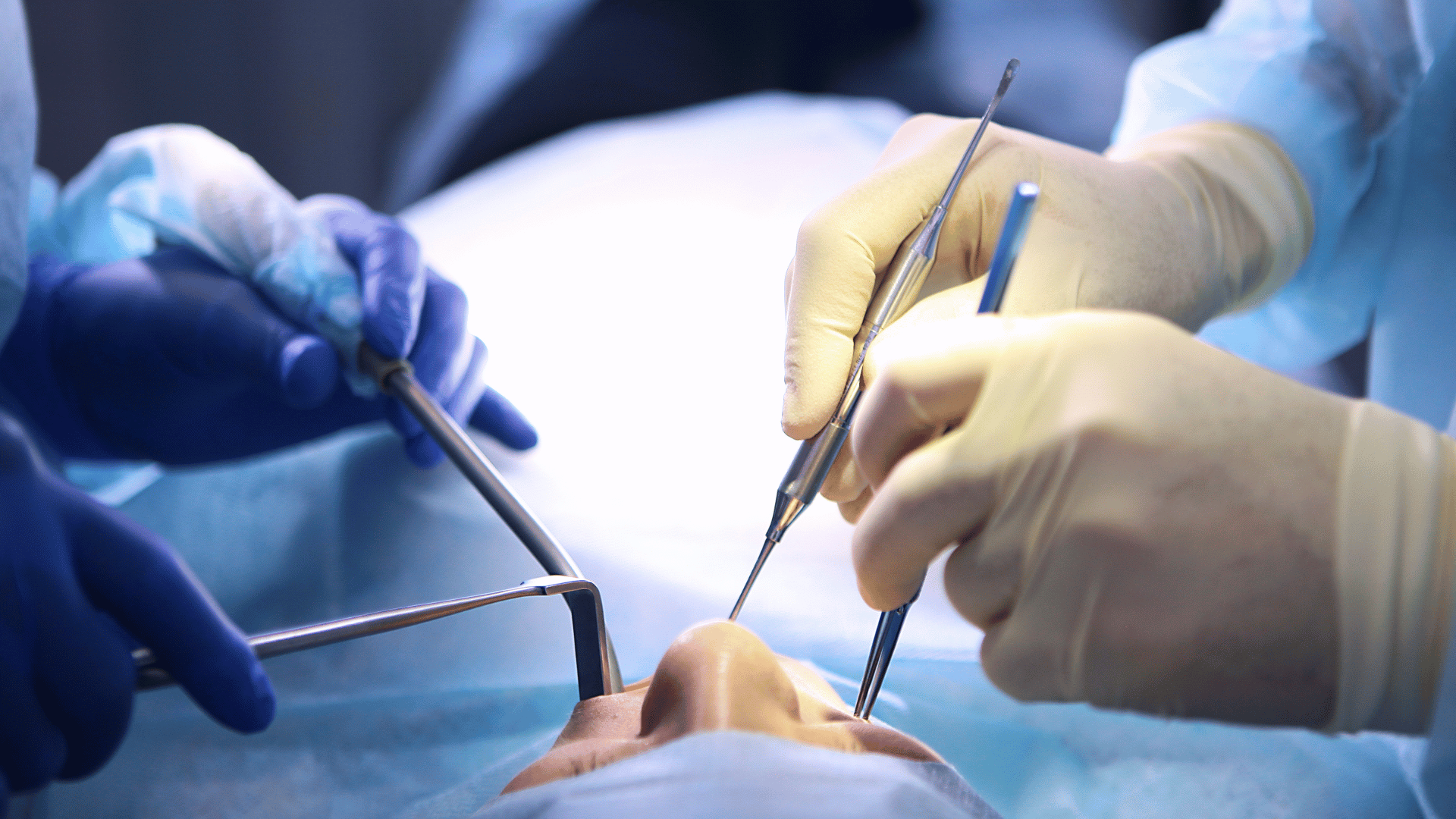
Chronic wounds are wounds that don’t heal after a few months, and over 6.5 million Americans experience them. Almost every wound contains bacteria; if it’s not detected and removed, it can lead to serious problems. For example, it could lead to serious infections, resulting complications, and sometimes amputation. When physicians clean out wounds, they remove bacteria. However, not all bacteria are visible to the human eye.
Chronic wounds are especially apparent in diabetic patients. They tend to develop diabetic foot ulcers (open sores); about one-third of people with diabetes suffer from them. According to the American Diabetes Association, about 20% of those who develop a foot ulcer will require an amputation.
New research from Keck Medicine of USC suggests there is a more effective way to detect bacteria when cleaning out a wound. This could help individuals with chronic wounds like diabetic foot ulcers.
Lighting Up Bacteria
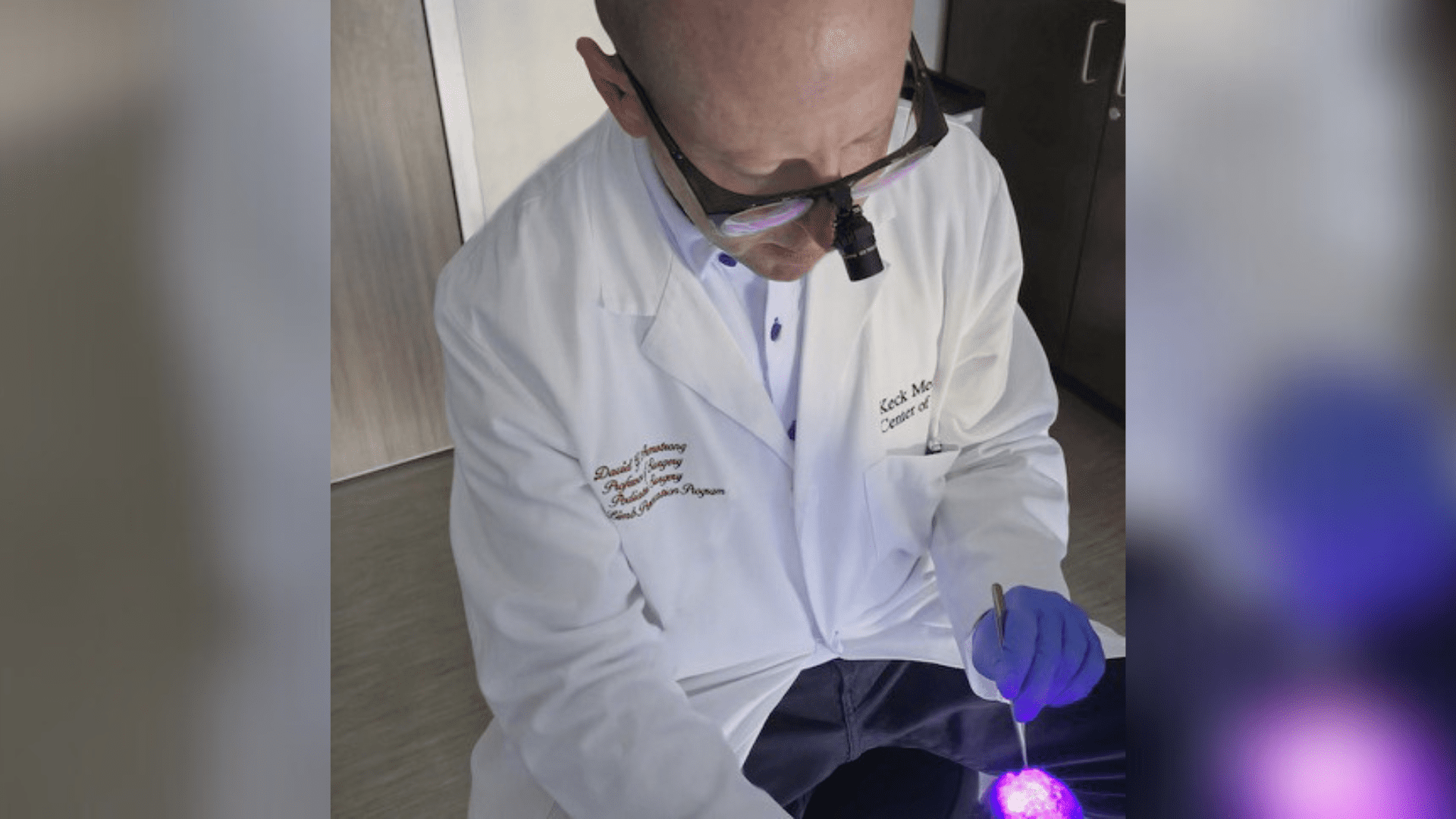
Autofluorescence (AF) imaging involves a handheld device “lighting up” bacteria that was once invisible to the human eye. It uses violet light to illuminate molecules in the cell walls of bacteria. Different types of bacteria turn different colors, which allows physicians to determine what kind and how much bacteria is in a wound.
“We’re hopeful this new technology can help surgeons improve their accuracy when pinpointing and consequently removing bacteria from wounds and therefore improve patient outcomes, particularly for those with diabetic foot wounds,” said Dr. David Armstrong, a podiatric surgeon with Keck Medicine and the study’s senior author. Dr. Armstrong, a limb preservation specialist, said, “The early detection and removal of bacteria from a wound is vital to preventing avoidable amputations.”
The research reveals that “AF imaging can identify bacteria in wounds in approximately 9 in 10 patients that traditional clinical assessments miss.”
Identifying Bacteria
Typically, when a physician debrides or cleans a wound, the samples are sent to a lab to specify the different types of bacteria. The lab determines the best treatment protocol, such as antibiotics or special wound dressings. However, this process can take several days, leaving the wound vulnerable to infection.
AF imaging allows physicians to make these decisions during the wound debridement rather than waiting for the lab results. In addition, if the bacteria is caught early, the patient can potentially avoid antibiotics. The benefit of avoiding antibiotics is the patient potentially avoids antibiotic resistance.
“This real-time intervention may allow for faster, more effective treatment for wounds,” said Armstrong. Keck Medicine physicians are currently using this technology to treat people with chronic wounds, such as diabetic foot ulcers.
“I look forward to more research in this area as we hope to see AF imaging become the standard of care for wound care in the near future,” said Armstrong.